Amyloid-β (Aβ) immunotherapy has recently begun to gain considerable attention as a potentially promising therapeutic approach to reducing the levels of Aβ in the Central Nervous System (CNS) of patients with Alzheimer's Disease (AD). Despite extensive preclinical evidence showing that immunization with Aβ(1-42) peptide can prevent or reverse the development of the neuropathological hallmarks of AD, in 2002, the clinical trial of AN-1792, the first trial involving an AD vaccine, was discontinued at Phase II when a subset of patients immunized with Aβ(1-42) developed meningoencephalitis, thereby making it necessary to take a more refined and strategic approach towards developing novel Aβ immunotherapy strategies by first constructing a safe and effective vaccine.
This review describes the rational basis in modern clinical trials that have been designed to overcome the many challenges and known hurdles inherent to the search for effective AD immunotherapies. The precise delimitation of the most appropriate targets for AD vaccination remains a major point of discussion and emphasizes the need to target antigens in proteins involved in the early steps of the amyloid cascade. Other obstacles that have been clearly defined include the need to avoid unwanted anti-Aβ/APP Th1 immune responses, the need to achieve adequate responses to vaccination in the elderly and the need for precise monitoring.
Novel strategies have been implemented to overcome these problems including the use of N-terminal peptides as antigens, the development of DNA based epitope vaccines and vaccines based on passive immunotherapy, recruitment of patients at earlier stages with support of novel biomarkers, the use of new adjuvants, the use of foreign T cell epitopes and viral-like particles and adopting new efficacy endpoints. These strategies are currently being tested in over 10,000 patients enrolled in one of the more than 40 ongoing clinical trials, most of which are expected to report final results within two years.
Summary of the main strategies and rational to overcome the challenges raised from the AN1792 clinical trial:
This review describes the rational basis in modern clinical trials that have been designed to overcome the many challenges and known hurdles inherent to the search for effective AD immunotherapies. The precise delimitation of the most appropriate targets for AD vaccination remains a major point of discussion and emphasizes the need to target antigens in proteins involved in the early steps of the amyloid cascade. Other obstacles that have been clearly defined include the need to avoid unwanted anti-Aβ/APP Th1 immune responses, the need to achieve adequate responses to vaccination in the elderly and the need for precise monitoring.
Novel strategies have been implemented to overcome these problems including the use of N-terminal peptides as antigens, the development of DNA based epitope vaccines and vaccines based on passive immunotherapy, recruitment of patients at earlier stages with support of novel biomarkers, the use of new adjuvants, the use of foreign T cell epitopes and viral-like particles and adopting new efficacy endpoints. These strategies are currently being tested in over 10,000 patients enrolled in one of the more than 40 ongoing clinical trials, most of which are expected to report final results within two years.
Ongoing clinical trials based on active or passive immunotherapy for AD.
NAME | FDA PHASE | MECHANISM OF ACTION |
ACC-001 | Phase II/IIa/IIb | ACC-001 is a short amino-terminal Aβ (1-6) fragment that is derived from the N-terminal B cell epitope of Aβ while avoiding T cell activation. Antibodies specific for this Aβ peptide can cross the blood-brain barrier and act directly in the central nervous system to induce plaque clearance. |
CAD-105 | Phase II | CAD-105 is Aβ1–5 coupled to Qb virus-like particles. Antibodies specific for this Aβ peptide can cross the blood-brain barrier and act directly in the central nervous system to induce plaque clearance. |
V950 | Phase I | V950 is an Aβ amino-terminal peptide conjugated to ISCO-MATRIX®. |
UB311 | Phase I | UB311 uses the peptide Aβ1–14 with UBITh®. The UBITh AD immunotherapeutic vaccine has been engineered to elicit anti-N-terminal Aβ (1-14) antibodies while minimizing potential for the generation of adverse anti-Aβ immune responses. The vaccine has been further designed for minimization of inflammatory responses through the use of a proprietary vaccine delivery system that favors Th2 type regulatory T cell responses over Th1 pro-inflammatory T cell responses. |
Affitope AD02 / Mimotope Aβ(1-6) | Phase II/IIa/IIb | Affitope AD02 is a short amino-terminal Aβ fragment (Aβ1-6) that is derived from the N-terminal B cell epitope of Aβ while avoiding T cell activation. |
AAB-001 / Bapineuzumab | Phase III | Bapineuzumab is an anti-Aβ antibody that binds specifically to soluble amyloid-β and therefore may act to draw the peptide away from the brain through the blood to be cleared in the periphery. |
CAD106 | Phase II/IIa/IIb | CAD106 is a vaccine based on an epitope that contains multiple copies of the Aβ 1-6 peptide, that avoids T cell activation, coupled to the Qβ virus-like particle. |
Intravenous Immunoglobulin /Gammagard, IVIg | Phase III | Intravenous Immunoglobulin (IVIg) is obtained from the pooled plasma of healthy human blood donors, and contains natural anti-amyloid antibodies. In vitro data have demonstrated that human anti-Aβ antibodies inhibit fibril formation and diminish neurotoxicity. |
MABT5102A | Phase I | MABT5102A is a humanized monoclonal antibody that binds Aβ. |
Solanezumab / LY2062430 | Phase III | Solanezumab binds specifically to soluble amyloid-β and therefore may act to draw the peptide away from the brain to be cleared in the periphery. |
PF-04360365 | Phase II | Multiple IV Dose Study of anti-Aβ mAb in patients with mild To moderate AD. PF-04360365 binds to Aβ. |
R1450 | Phase II | R1450 is a fully humanized monoclonal antibody that binds Aβ. |
GSK933766A | Phase I | Anti-Aβ antibody that binds Aβ. |
Summary of the main strategies and rational to overcome the challenges raised from the AN1792 clinical trial:
Strategy | Rational |
Challenge: Unwanted anti-Aβ/APP Th1 immune responses | |
Using N terminal peptide (Ab1–15) as antigen | The Ab1–15 peptide is the major B cell epitope. Antibodies raised to amino acids 1–11, 1–7, and 1–5 of Ab42 bind to b-amyloid plaques with higher affinity and initiate immune responses much stronger than antibodies raised to amino acids 3–7, 5–11, and 11–26. The smallest domain in the Ab peptide to which the antibodies bind with high affinity is that encoding amino acids 4-10. |
Using DNA based epitopes | DNA-based vaccination induces prolonged, endogenous antigen synthesis and processing within the subject’s own cells infected with virus encoding the desired epitopes and adjuvants. Adjuvants facilitate the internalization of antigen into the antigen presenting cells to enhance the efficiency of processing and presentation of the antigens. |
Using new adjuvants | Mannan is as a potentially optimal molecular adjuvant due to its ability to enhance both B- and T-cell immune responses. This adjuvant has the advantage of inducing a Th2 rather than Th1 response |
Using passive immunotherapy | Vaccines using monoclonal antibodies or Immunoglobulins do not show adverse reactions related to cellular immunity |
Challenge: The need of early treatment | |
Early diagnosis with support of biomarkers | Repeated vaccination at regular intervals since early stages would increase the probability of a good response before the toxic forms of β-amyloid begin to accumulate. |
Challenge: Hypo-responsiveness to vaccines in the elderly | |
Recruiting previously generated memory T cells | A vaccine based on Ab peptide fused with Th epitopes from conventional vaccines or common pathogens produced during childhood vaccination or during prior exposure to human pathogens could potentially induce a rapid expansion of pre-existing memory T cells and their differentiation into effector T cells |
Using Foreign T cell epitope | Foreign T cell epitopes as synthetic, non-natural Pan HLA DR-binding epitopes produce more potent responses on a molar basis than a tetanus-derived universal epitope. |
Using Viral-like particles | Incorporation of the Ab B cell epitope into a viral capsid protein allows the expression of this epitope on the surface of VLP in a repetitive and ordered array. Such organization of the epitope may induce T cell-independent B cell activation and production of high titers of anti-Ab antibodies |
Challenge: The need of more precise monitoring | |
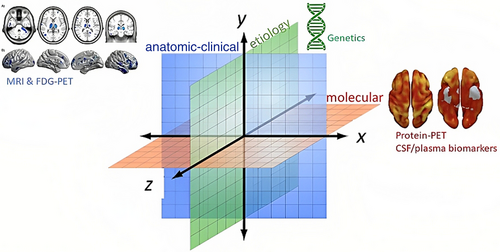
Adopting new efficacy endpoints | Besides traditional endpoints, new clinical endpoints such as neuroimaging and biomarkers provide a more detailed picture of basal status and response of the patients. |